Before sending claims
You may need to complete the following steps before sending claims.Transaction enrollment
All payers require providers to complete an enrollment process before they can start receiving 835 ERAs. Some payers also require enrollment before allowing providers to submit claims. The Stedi Payer Network lists which payers require transaction enrollment. Visit Transaction Enrollment for details about the transaction enrollment process.Coordination of benefits check (recommended)
We recommend running a coordination of benefits (COB) check to ensure you submit claims to the correct payer. COB checks can help you determine:- If a patient is covered by more than one health plan
- Whether coverage overlap requires coordination of benefits
- Each payer’s responsibility for payment (primacy) in coordination of benefits scenarios
SFTP submission
You can use Stedi’s fully-managed SFTP server to submit claims to to payers and retrieve claim responses without calling Stedi’s APIs. You must submit claims in X12 EDI format, and Stedi returns claim responses through the SFTP connection in X12 EDI format. This makes Stedi SFTP a good option if you have an existing system that generates X12 EDI files and you want to send them through the Stedi clearinghouse without completing an API integration. Visit SFTP connection for more information.API submission
Call the Institutional Claims endpoint to submit 837I institutional claims in JSON. The endpoint returns a synchronous response from Stedi in JSON format. Later, Stedi will respond with a 277CA claim acknowledgment, and the payer will respond with both 277CAs and the 835 ERA.Headers
When constructing the request, you must include the following information in HTTP headers:Authorization: Generate an API key to use for authentication.Content-Type: Set toapplication/json.
Body
The information you submit for a claim depends on your use case. Refer to the Institutional Claims endpoint for a complete list of properties. However, all claims require the following high-level information:| Information | Description | |
|---|---|---|
tradingPartnerServiceId | This is the payer ID. Visit the Payer Network for a complete list. | |
submitter object | Information about the entity submitting the claim. This is an organization, such as a hospital or other treatment center. | |
receiver object | Information about the entity responsible for the payment of the claim, such as an insurance company or government agency. | |
subscriber and/or dependent objects | Information about the patient who received the medical services. Note that if a dependent has their own, unique member ID for their health plan, you should submit their information in the subscriber object and omit the dependent object from the request. You can check whether the dependent has a unique member ID by submitting an Eligibility Check to the payer for the dependent. The payer will return the member ID in the dependents.memberId field, if present. | |
claimInformation object | Information about the claim, such as the claim filing code (identifies the type of claim), claim charge amount, and place of service code. It also includes information about each individual service line included in the claim. | |
| Billing provider | You must supply information about the billing provider in either the providers or billing object. This includes the provider’s NPI, name, and other information. |
Service line identification
A claim can contain multiple service lines. Since the payer may accept, reject, or pay a subset of those lines, you can receive an 835 ERA that references apatientControlNumber, but only pertains to some of the service lines.
However, the claimInformation.serviceLines.lineItemControlNumber serves as a unique identifier for each service line in your claim submission. This value appears in the 277CA claim acknowledgment and 835 ERA as the lineItemControlNumber, allowing you to correlate these responses to specific service lines from the original claim. We strongly recommend setting the lineItemControlNumber to a ULID or other unique identifier for each service line. We recommend using a ULID instead of a UUID because the property has a max of 30 characters.
Conditional requirements
Note that objects marked as required are required for all requests, while others are conditionally required depending on the circumstances. When you include a conditionally required object, you must include all of its required properties. For example, you must always include thesubscriber object in your request, but you only need to include the supervising object when the rendering provider is supervised by a physician.
Character restrictions
Only use the X12 Basic and Extended character sets in request data. Using characters outside these sets may cause validation and HTTP400 errors.
Basic character set
Basic character set
The X12 Basic character set includes uppercase letters, digits, space, and some special characters. Lowercase letters and special language characters like 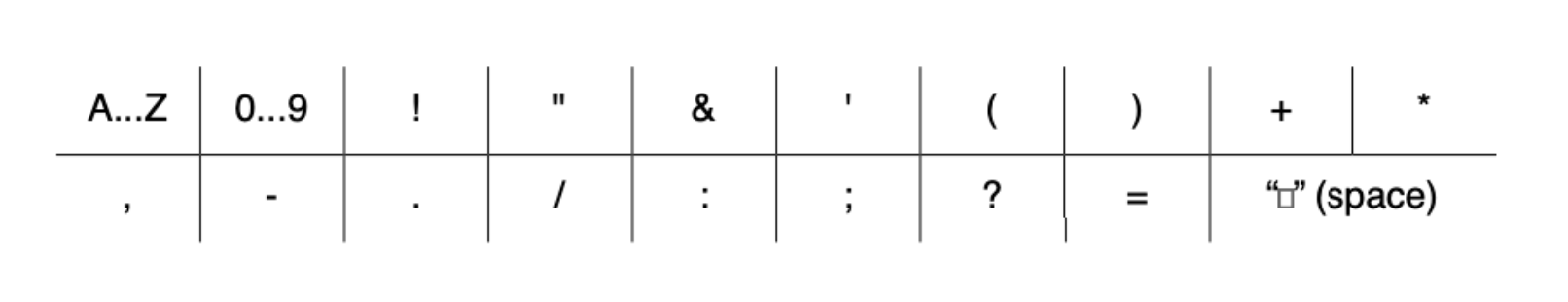
ñ are not included.The following special characters are included: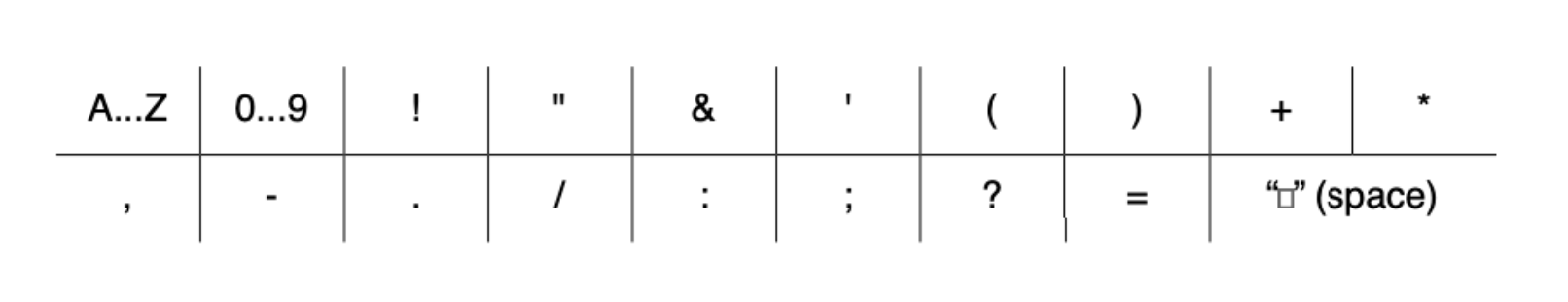
Extended character set
Extended character set
The Extended character set includes the characters listed in Basic, plus lowercase letters and additional special characters, such as 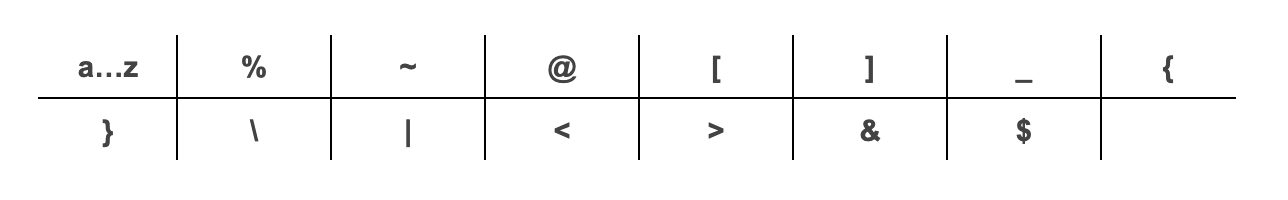
@.The following additional special characters are included:
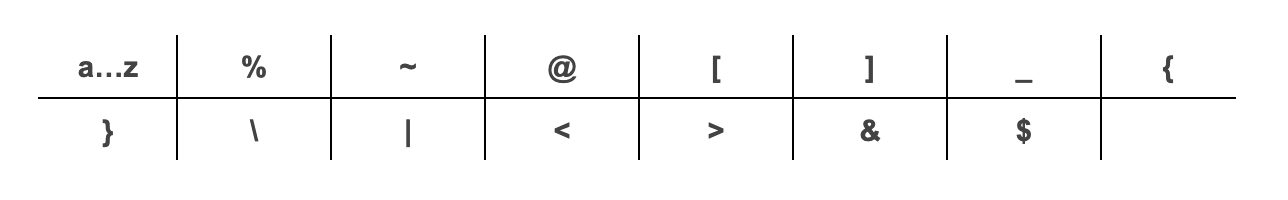
~, *, : and ^. They are reserved for delimiters in the resulting X12 EDI transaction, and X12 doesn’t support using escape sequences to represent delimiters or special characters. Stedi returns a 400 error if you include these restricted characters in your request.
Sample request and response
The following example sends an institutional claim. The response shape contains summary information from Stedi about the claim submission and whether it was successful.Test claims
All claims you submit through the API are sent to the payer as production claims unless you explicitly designate them as test data. To send test claims:- JSON endpoint: Set the
usageIndicatorproperty in the test claim body toT. - X12 EDI endpoint: Set
ISA15(Interchange Usage Indicator) toT(Test Data) instead ofP(Production Data).
Recommended API clients
You may want to use an API client to make testing and debugging easier. We don’t recommend using Postman for requests containing Protected Health Information (PHI) because Postman defaults to storing request history - including full request payloads - on its cloud servers. You can’t turn this feature off without impractical workarounds. Visit API clients for a list of recommended clients you can use instead.Claim Filing Indicator Code
The Claim Filing Indicator Code indicates how a claim was filed with a payer, such asMC (Medicaid) or CI (Commercial Insurance Co.).
Choosing the correct claim filing indicator code is important for successful claim submission. Visit the Claims code lists documentation for best practices for selecting the appropriate code.
275 claim attachments
If the claim requires attachments, you must include additional details about the attachments in the appropriate objects:- Attachments for entire claim:
claimInformation.claimSupplementalInformation.reportInformation - Attachments for a specific service line:
claimInformation.serviceLines.serviceLineSupplementalInformation
Cancel or resubmit claims
You may need to resubmit claims for several reasons, including changes to the patient’s coverage, errors in the original claim’s information, or appealing a denied claim. You may also need to cancel duplicate claims or claims that were submitted in error. We recommend the following for resubmitting or canceling claims:- Correct or replace claims: Set
claimInformation.claimFrequencyCodeto7- Replacement of Prior Claim. We also recommend setting a new, uniquepatientControlNumber. The payer includes this value in their 835 ERA, allowing you to easily correlate that response with your resubmission. - Cancel claims : Set
claimInformation.claimFrequencyCodeto8- Void/Cancel of Prior Claim.
claimInformation.claimSupplementalInformation.claimControlNumber to the Payer Claim Control Number (sometimes called the ICN). This is different from the patientControlNumber you sent in the claim and the Stedi-generated controlNumber returned in the API response. You can retrieve the Payer Claim Control Number from one of the payer’s 277CA claim acknowledgments in the transactions.payers.claimStatusTransactions.claimStatusDetails.patientClaimStatusDetails.claims.claimStatus.tradingPartnerClaimNumber property.
Submit claims to a secondary or tertiary payer
In coordination of benefits (COB) scenarios, you’ll need to submit a claim to multiple payers. You must set thesubscriber.paymentResponsibilityLevelCode to either S (when submitting to the secondary payer) or T (when submitting to the tertiary payer).
You must also include the following information about how prior payers have adjudicated the claim. For example, if a patient’s private insurance plan (primary payer) adjusted the requested reimbursement amount and paid for its portion of the services, you must include that information in the claim you submit to Medicare (secondary payer). You can find these details in 835 ERA responses from prior payers.
Claim information
You must submit oneclaimInformation.otherSubscriberInformation object for each prior payer. Supply all the required properties in the object plus the following additional information:
claimLevelAdjustments: Provide if the prior payer made adjustments at the claim level. Codes and their associated amounts must come from ERAs sent by the prior payers. You can find these codes in the ERA’stransactions.detailInfo.paymentInfo.claimAdjustmentsobject.medicareInpatientAdjudication(institutional claims only): You must include this if Medicare was one of the prior payers and reported inpatient adjudication information on the ERA.medicareOutpatientAdjudication: You must include this if Medicare was one of the prior payers and reported outpatient adjudication information on the ERA.otherPayerName.otherPayerAdjudicationOrPaymentDate: The date the payer adjudicated or paid the claim. You must provide this if you aren’t providing a value in theclaimInformation.serviceLines.lineAdjudicationInformation.adjudicationOrPaymentDateproperty.payerPaidAmount: This is the total amount in dollars the payer paid on this claim.
Service line information
You must submitserviceLines.lineAdjudicationInformation objects when the prior payers provided line-level adjudication information. Submit one object for each prior payer. For each object, you should include the following properties.
adjudicationOrPaymentDate: The date the payer adjudicated or paid the claim. Don’t include this if you’re providing a date in theotherPayerName.otherPayerAdjudicationOrPaymentDateproperty.claimAdjustmentInformation: You can find this information in the ERA’stransactions.detailInfo.paymentInfo.serviceLines.serviceAdjustmentsobject.otherPayerPrimaryIdentifier: The identifier for the other payer. This value should match the identifier you supplied for the payer in theclaimInformation.otherSubscriberInformation.otherPayerName.otherPayerIdentifierproperty.procedureCode: The adjudicated procedure code for the service line.serviceIdQualifier: A code identify the type of procedure code. Visit Claims code lists for a complete list.serviceLinePaidAmount: The total amount in dollars the prior payer paid on this service line.paidServiceUnitCount: The number of paid units for the service line. When paid units are not present on the remittance advice, use the original billed units.remainingPatientLiability: The amount of the service line the patient is responsible for paying.

